In its 2016 study, the World Health Organization reported that an estimated 422 million people worldwide suffer from diabetes. The number has more than quadrupled over the past 40 years. As a result, instances of diabetes-related complications such as diabetic retinopathy have similarly skyrocketed.
According to the National Eye Institute, the condition is the most common cause among adults of new cases of blindness or significant visual impairment. As such, research into the condition is being carried out tirelessly, both in the USA and globally. Here, we take a look at two of the latest developments.
Diabetic retinopathy is one of the cruelest potential consequences of diabetes: if left untreated, it can lead to loss of sight. The condition occurs when high blood sugar levels, raised blood pressure and high lipid levels damage the blood vessels leading to the retina. By 2030, it could become the leading cause of blindness worldwide. Although diabetes rates are soaring in many countries, the prevalence of diabetic retinopathy in the Virgin Islands and the Caribbean, in general, is almost fifty percent higher than the global average.
While scientists struggle to identify the precise reasons for this high incidence of diabetes, Caribbean countries must address the health, social and economic consequences. The economies of the region are small and undiversified, the climate tropical and the countries vulnerable to natural disasters and economic shocks. Population growth is high, and poverty and inequality persist. The diabetes burden places additional strain on already limited health care resources. Few nation-wide integrated approaches to the treatment of diabetic retinopathy exist.
Early diagnosis by smartphone
In this information age, we turn to our smartphones to answer most of life’s questions, from the weather forecast to the sports news to where we can get the best insurance deal. But could our beloved phones even help with a diagnosis for our patients with diabetic retinopathy in Virgin Islands?
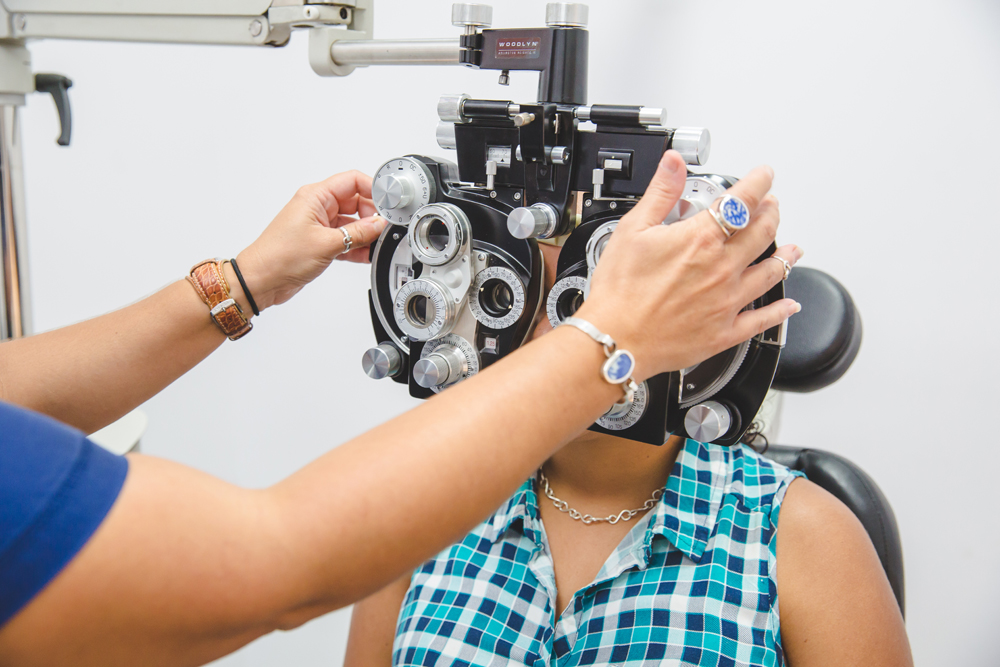
Researchers in India have developed software that can do just that. With any medical condition, early diagnosis is key to the best possible outcome, and at present, those with diabetes are subjected to retinal screening using an ophthalmoscope.
As instances of diabetes continue to rise, this is putting ever more pressure on resources, particularly in parts of the world where the medical infrastructure is less developed. Consequently, months can pass between the initial diagnosis and the appropriate retinal screening.
The new technology uses Artificial Intelligence (AI) to analyze retinal images taken directly by your smartphone and has been found to be highly useful in detecting diabetic retinopathy. The trial assessed 300 patients and compared the findings of the AI with that of qualified ophthalmologists. The results were very close, with the software making 203 positive diagnoses compared to 191 from the medical experts.
A bright future
The research brings genuine hope to Plessen’s patients who are fighting diabetic retinopathy in Virgin Islands and of course to sufferers across the globe. These are just two examples of the cutting edge work taking place in the fight to improve the plight of those at risk, regarding prevention, diagnosis and, most important of all, treatment.
Plessen’s diabetic retinopathy treatment in St. Thomas and St. Croix takes advantage of every new advance in technology, and while both these areas of research still need significant development before they can be put to wider use, they represent genuine areas of hope for a brighter future.