Written by Dr. Jonathan Leon Rosen
Daily blood sugar testing has been the hallmark for diabetes control for decades. However, it may not be the best representative of the patient’s long-term sugar control. For example, a patient with blood sugars in the 400s starts taking their insulin and now has sugar levels in the 120s. When asked by the doctor’s staff, the patient only reports the lower level of sugar, inadvertently giving a false sense of control and increasing the risk of conditions such as diabetic retinopathy developing.
To combat this, Hemoglobin A1C levels can be used to get a clearer picture of the patient’s overall control of their sugar. Hemoglobin A1C (HgbA1C) measures the changes that the elevated blood sugar creates within the patient’s Red Blood Cell’s hemoglobin. These changes can be used as an indirect measure of the changes that Diabetes causes in the patient’s tissues, which lead to the various maladies of diabetes such as neuropathy or retinopathy.
These changes in the hemoglobin last the life cycle of the red blood cell which is approximately 3 to 4 months. As such, Hemoglobin A1C is checked two to four times per year depending on the patient’s diabetes control. Various conditions such as sickle cell disease or G6PD deficiency can artificially lower the HgbA1C level. As such, patients should check with their medical doctor to see if other medical conditions are affecting their HgbA1C levels.
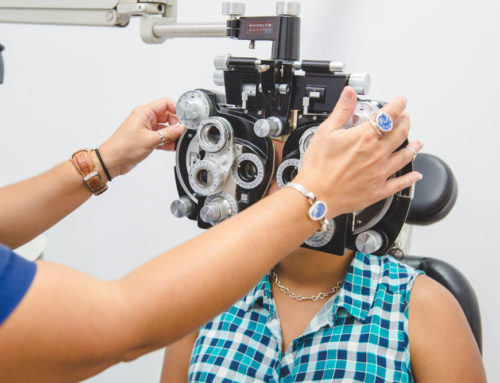
Diabetic retinopathy occurs when a patient’s blood sugar levels are uncontrolled over an extended period of time. As a malady that manifests in the eye, your ophthalmologist is often the first person to be alerted that something is wrong, and Plessen’s ophthalmologist in Virgin Islands has seen numerous cases over the years.
These elevated levels cause the capillaries of the retina to become leaky and frail. This leads to bruising and thickening of the retina with eventual deposits of cholesterol called exudates. When this thickening occurs in the central part of the retina, the Macula, the vision tends to worsen quickly. As the effects of the diabetes builds, the retina develops a low oxygen level and begins to develop new abnormal blood vessels; a process called neovascularization.
Neovascularization of the retina can quickly develop into neovascularization of the rest of the eye. When this happens, the pressure of the eye can go up, pain can occur, bleeding inside the eye can happen, among other issues. If not treated promptly, it can quickly lead to blindness. Even when treated quickly, long term problems with pressure of the eye and scarring can occur.
Diabetic Retinopathy can be seen in patients with any level of Hemoglobin A1C, however, it is more likely to be seen in patients with a HgbA1C greater than 7.0. The higher the HgbA1C, and the longer it is sustained at that higher level, the higher the likelihood of developing diabetic retinopathy. Other factors such as a patient’s blood pressure can also affect the chance of developing retinopathy.
If you are diabetic, you should ask your medical doctor about your Hemoglobin A1C levels. You should also be evaluated by one of Plessen’s Ophthalmic Care providers to assess your level of diabetic retinopathy.
For evaluations in St. Thomas, call 340-774-2015 to make an appointment.
For evaluations in St. Croix, call 340-773-2015 to make an appointment.