Diabetic retinopathy is the most common cause of blindness in the 24 to 70 year age group.
Diabetes affects not only the blood sugar level but also causes damage to small blood vessels throughout the body. These changes occur very gradually and become more common as a person has had diabetes for a longer period of time. Because a person with early diabetes may have no symptoms, one may have had the disease for several years before it is diagnosed.
With time, the circulation to the kidneys, the peripheral nerves, the feet, the heart, and the eyes are especially affected. If you have numbness, tingling, or loss of sensation in the feet, it is likely that you are beginning to have what is referred to as peripheral neuropathy. This means there is damage to peripheral nerves from reduced blood supply. Often when a person has neuropathy, he or she may have diabetic retinopathy as well.
Initially, people do not experience pain or discomfort when living with retinopathy. By the time symptoms develop, the degree of retinal damage can be quite extensive. If you are diabetic, the American Academy of Ophthalmology recommends that you have your eyes dilated with drops and the retina examined at least annually.
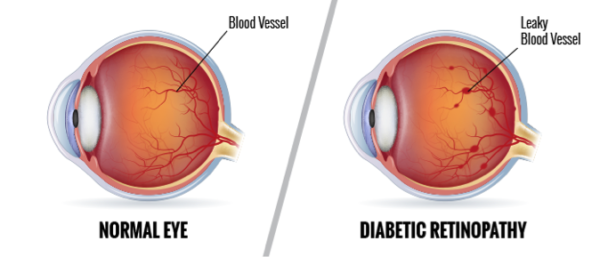
There are two basic stages of diabetic retinopathy. These are “background,” or “non-proliferative” diabetic retinopathy (NPDR) and “proliferative” diabetic retinopathy (PDR). The non-proliferative form is the earlier form, and the proliferative stage is the more advanced stage. The “proliferation” refers to the growth of abnormal new blood vessels, which grow in the back of the eye, like weeds, where they’re not supposed to grow. These blood vessels are weak, and can break and bleed, causing vitreous hemorrhage, and “floaters.” That is, spots floating in the vision. If the bleeding is more severe, the entire inside of the eyeball can be filled with blood, partially or totally blocking vision.
In the non-proliferative forms, the small capillaries in the back of the eyes develop tiny bulges called microaneurysms. In these spots, the walls of the vessels are weakened, and they leak a clear plasma-like fluid. This may make the retina wet and swollen, a condition known as “edema.” If the center of the retina is affected, as it usually is, the condition is known as macular edema.
Treatment
Macular edema can often be helped with a treatment known as focal laser treatment, to attempt to seal off the leaky points. When the leakage is more diffuse, sometimes a grid pattern of laser treatment is done. Laser eye surgery is a non-invasive form of treatment done in the office in which there are no incisions or cutting, no stitches and usually no anesthesia, other than an eye drop. This type of treatment results in an improvement in vision about 20-25% of the time, but mostly is intended to stabilize the situation, and reduce the likelihood that the vision will worsen.
The proliferative form of the disease is treated with a different kind of laser eye surgery, known as panretinal photocoagulation (PRP). This treatment involves a greater number of applications and is sometimes done in two or three separate sessions. The peripheral portion of the retina is treated, which can cause side effects such as constriction of visual field, as well as reduction in night vision. These side effects are relatively uncommon, and when they occur, are necessary tradeoffs to attempt to preserve the central vision.
In the event that there is severe hemorrhage into the vitreous (the clear gel that fills the central cavity of the eye), surgery can be done to remove the vitreous jelly, and the blood. This is known as vitrectomy surgery. This type of surgery may also be required if the abnormal blood vessels in the back of the eye form scar tissue, which pulls on the retina. This scar tissue may pull hard enough to lift the retina off the back of the eye like a tent. This situation is called a tractional retinal detachment.
There are some drugs that can be injected into the eye that are beneficial to those with diabetic macular edema, and in proliferate diabetic retinopathy. Current studies are underway that will bring to market newer medications that can be injected into the eye to help reduce or resolve diabetic macular edema.
With education, careful follow up, and tight management of the blood sugar, as well as early laser treatment when needed, most blindness from diabetes can be prevented.
